Helsingor Castle (the setting for Shakespeare’s Hamlet)
Dateline: May 8th, 2010, Helsingor, Denmark
This weekend I’m in Denmark doing a two-day workshop on “Supershrinks” sponsored by Danish psychologist and ICCE Senior Associate and Trainer Susanne Bargmann. Just finished the first day with a group of 30 talented clinicians working diligently to achieve their personal best. The challenge, I’m increasingly aware, is sustaining a commitment to seeking client feedback over time once the excitement of a workshop is over. On the surface, the idea seems simple: ask the consumer. In practice however, it’s not easy. The result is that many practitioners who are initially enthusiastic lose steam, eventually setting aside the measures. It’s a serious concern given that available evidence documents the dramatic impact of routine outcome and alliance monitoring on outcome and retention in behavioral health.
Support of like-minded colleagues is one critical key for sustaining commitment “after the thrill is gone.” Where can you find such people? As I blogged about last week, over a thousand clinicians are connecting, sharing, and supporing each other on the web-based community of the International Center for Clinical Excellence (If you’re not already a member, click here to request your own personal (and free) invitation to join the conversation).
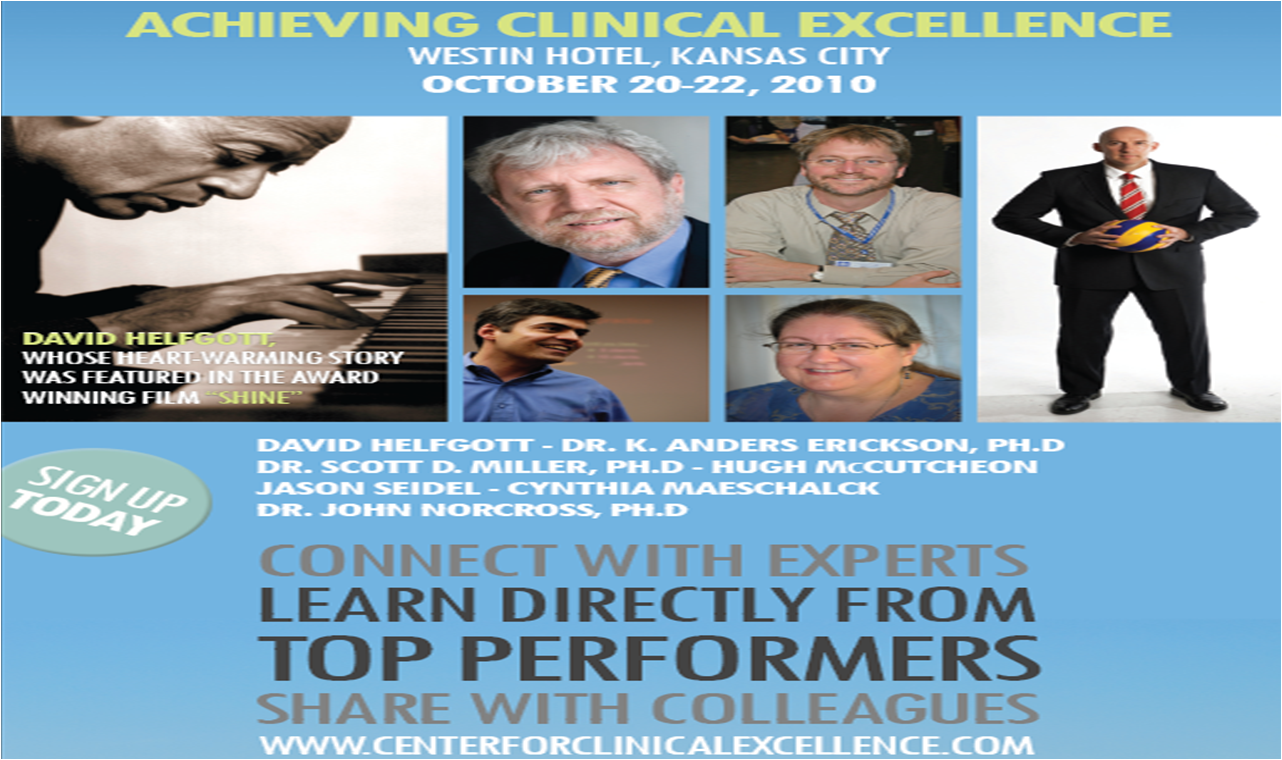
In the brief interview above, Susanne identifies a few additional steps that practitioners and agencies can take for making the process of seeking feedback successful over the long haul. By the way, she’ll be covering these principles and practices in detail in an afternoon workshop at the upcoming Achieving Clinical Excellence conference. Don’t miss it!

.png)




.gif)










.jpg)
.jpg)

.jpg)