The idea that improvement in a given skill or performance domain depends on practice is hardly new. Indeed, references to enhancing a person’s abilities through focused concentration and effort date back more than two millennia (1).
The idea that improvement in a given skill or performance domain depends on practice is hardly new. Indeed, references to enhancing a person’s abilities through focused concentration and effort date back more than two millennia (1).
Though the term, deliberate practice, includes the word, “practice,” it is altogether different. The goal is neither proficiency nor mastery. Rather, it is all about continuously reaching for objectives that lie just beyond one’s current ability.
Research and experience both confirm that the idea of using deliberate practice to improve therapeutic effectiveness is more appealing than the reality. Plainly put, it’s hard work. For most, once a modicum of proficiency has been achieved, interest in further improvement wanes (2). Moreover, as our confidence increases – generally far outstripping actual, measured ability — most seek out something more stimulating.
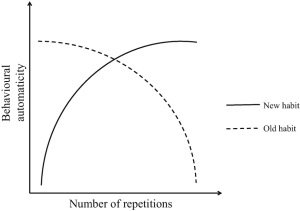
To be sure, it is not solely a question of motivation or will power. Being hardwired for novelty, the brain naturally selects and rewards the “new and different” (3). And, sadly, much in the professional development environment conspires with our biology to undermine continued effort. Talk of fresh, exciting discoveries, cutting-edge research, and improved theories and methods is constant and inescapable, all breathlessly reported. The underlying promise? The “state-of-the-art” is one workshop or certification away.
What to do?
Here are two helpful resources for using deliberate practice to improve your therapeutic effectiveness. The first is available for free thanks to the generosity of the University of New South Wales. In the video of his keynote address (below) for the Clinical Psychology program, my colleague and co-researcher, Dr. Daryl Chow, tackles the issue of novelty noted above, describing what it takes to develop a sustainable program of deliberate practice. Near the end, he talks about 4 different types of learners, identifying the one most likely to succeed. That said, the entire video is well worth watching.
 The second is the launch of the next online, asynchronous deliberate practice training. It’s entirely self-paced, delivering bite-sized nuggets twice a week specifically designed to help you stay focused and moving forward. You also become part of a growing learning community, connecting virtually with practitioners from around the world for guidance, support, and encouragement. To learn more or register, click here.
The second is the launch of the next online, asynchronous deliberate practice training. It’s entirely self-paced, delivering bite-sized nuggets twice a week specifically designed to help you stay focused and moving forward. You also become part of a growing learning community, connecting virtually with practitioners from around the world for guidance, support, and encouragement. To learn more or register, click here.
OK, that’s it for now. All the best,
Scott
Scott D. Miller, Ph.D.
Director, International Center for Clinical Excellence






























 ose not to go to psychotherapy because they are busy doing something else–consulting psychics, mediums, and other spiritual advisers–forms of healing that are a better fit with their beliefs, that “sing to their souls.”
ose not to go to psychotherapy because they are busy doing something else–consulting psychics, mediums, and other spiritual advisers–forms of healing that are a better fit with their beliefs, that “sing to their souls.”


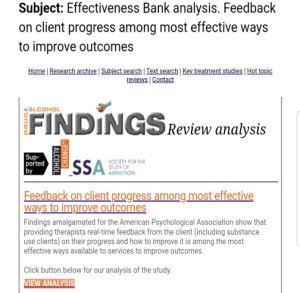
 associated with self-assessment, we actively work to limit information that conflicts with how we prefer to see ourselves (e.g., capable versus incompetent, perceptive versus obtuse, intuitive versus plodding, effective versus ineffective, etc.).
associated with self-assessment, we actively work to limit information that conflicts with how we prefer to see ourselves (e.g., capable versus incompetent, perceptive versus obtuse, intuitive versus plodding, effective versus ineffective, etc.).







.jpg)
.jpg)

.png)









.jpg)
.jpg)
.jpg)