I entered university an accounting major.
My first year, I took all the recommended courses: accounting theory, fundamentals of financial and managerial accounting, and so on.
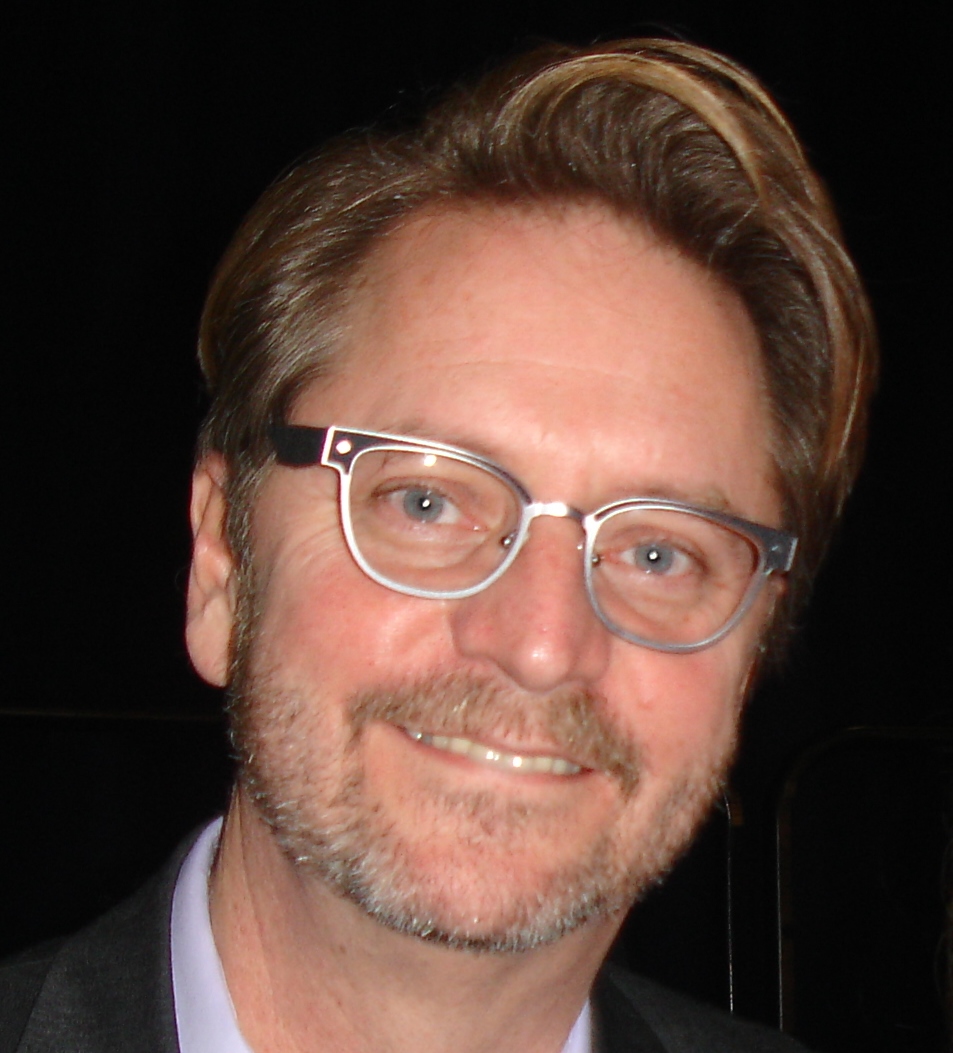
I’d likely be sitting in an office balancing company ledgers or completing tax documents had I never met Hal Miller. A Harvard-educated professor, Dr. Miller taught multiple sections of the Psychology 111 course students could take as part of the required “general education” curriculum.
Decades have now passed since I first met him. Still, I remember that first class as if it were yesterday. When I arrived, every seat in the large, theater-style classroom was already taken, students overflowing into the hallway outside. In time, I’d learn many were not officially registered for the class. They were there because they wanted to hear him speak.
Within weeks, I’d changed my major to psychology. I’m not sure how interested I was in the subject at the time. Rather, I wanted to be like Hal Miller. He loved what he was doing, was devoted to learning, and, most importantly, made me want to study. He was, in a word, charismatic.
“Charisma,” researchers Antonakis, Fenley, and Liechti report, “is rooted in values and feelings. It’s influence born of the alchemy that Aristotle called, the logos, the ethos, and the pathos.”
LOGOS = WORDS, LOGIC, FACTS
ETHOS = ETHICS, CREDIBILITY, EXPERTISE
PATHOS = EMOTIONS, CONNECTION, LIKE-MINDEDNESS
Hal Miller embodied all three qualities. His ability to engage, communicate, and inform, literally changed my life. I’m sure you can identify people who’ve had a similar impact on you.
But how did he do what he did? Did he learn it? Was it in his genes?
It turns out, the word, charisma, comes from the Greek χάρισμα, meaning “gift of grace” — a view widely held even today. You either “got it or you ain’t.”
Curiously, while one study in psychotherapy found it to be both relationally and therapeutically helpful, most of the serious research on the subject comes from other fields where social influence is critical to success (e.g., leadership, training, management). There, the evidence is clear: charisma is, “a learnable skill or, rather, a set of skills,” the potency of which can be dramatically improved with practice.
What exactly does that entail?
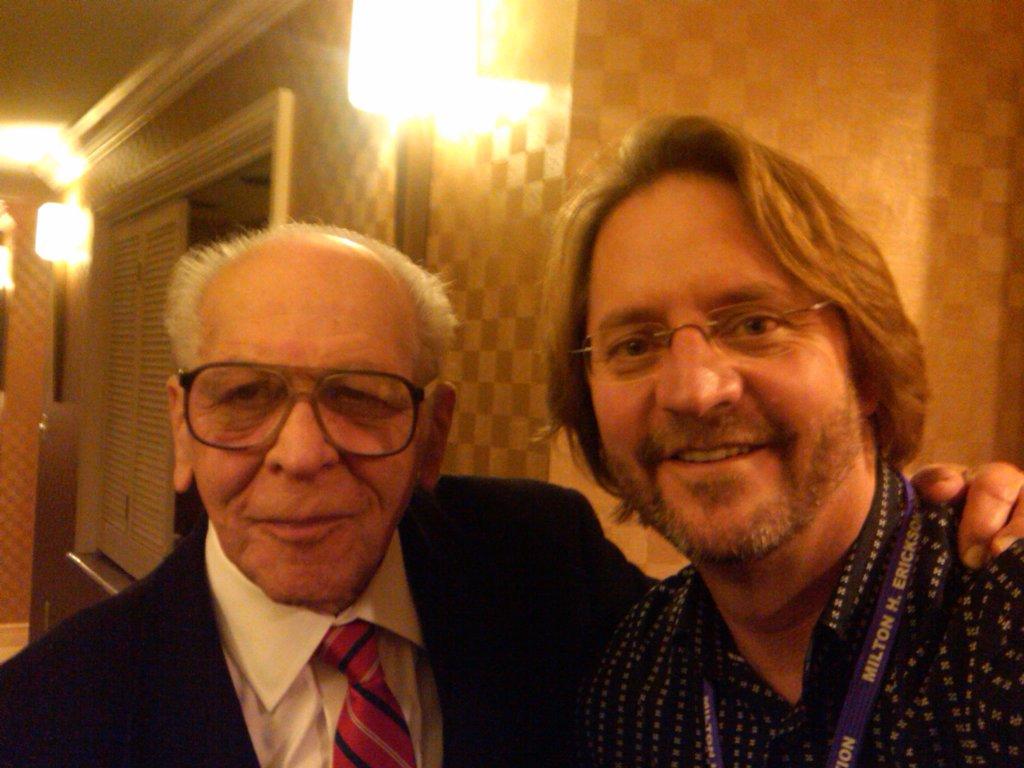
As a person whose spent his entire professional career providing continuing education workshops to therapists, I can tell you the absence of specific training means its mostly trial and error. A few have the good fortune to work closely with a gifted practitioner or presenter. I had the opportunity, or example, to work closely with Insoo Berg — a person who exuded warmth and charisma both in the therapy room and on the lecture circuit. And yet, rarely are students of charismatic individuals are as successful or magnetic as their mentors.
So, what does it take?
As hackneyed as it may sound at first, the key is “being yourself.” While its tempting to copy the content, style, and mannerisms of the Hal Millers and Insoo Bergs in our lives, doing so, everyone quickly recognizes, is mere tribute. Success means putting the principles of charisma — logos, ethos, pathos — into practice in a way that is congruent with who you are, your own style, persona and, critically, message.
Below, you’ll find a TedTalk by Professor John Antonakis, one of the leading researchers on charisma. It’s worth a listen. The first 5 minutes is interesting and provocative, but you must listen longer to learn about the evidence documenting that you can dramatically improve your ability to communicate with impact.
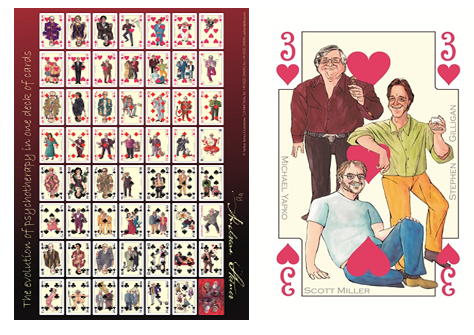
If you still are looking for something more practical and skill-based, and specific to psychotherapy, then join my colleagues and I for the “Training of Trainers” workshop, held once every other year. Together with an international faculty, and participants from around the world, we’ll work on helping you become the most effective version of you, either in your role as a therapist or trainer/presenter.




 with his story. Then, he played—doing with one hand what many would think impossible with two. When asked what drove him to continue in the face of so many challenges, he said, in a quiet yet confident voice, “Because there is so much to learn!”
with his story. Then, he played—doing with one hand what many would think impossible with two. When asked what drove him to continue in the face of so many challenges, he said, in a quiet yet confident voice, “Because there is so much to learn!”









.jpg)
.jpg)
.jpg)
.png)
.jpg)


.jpg)
.jpg)