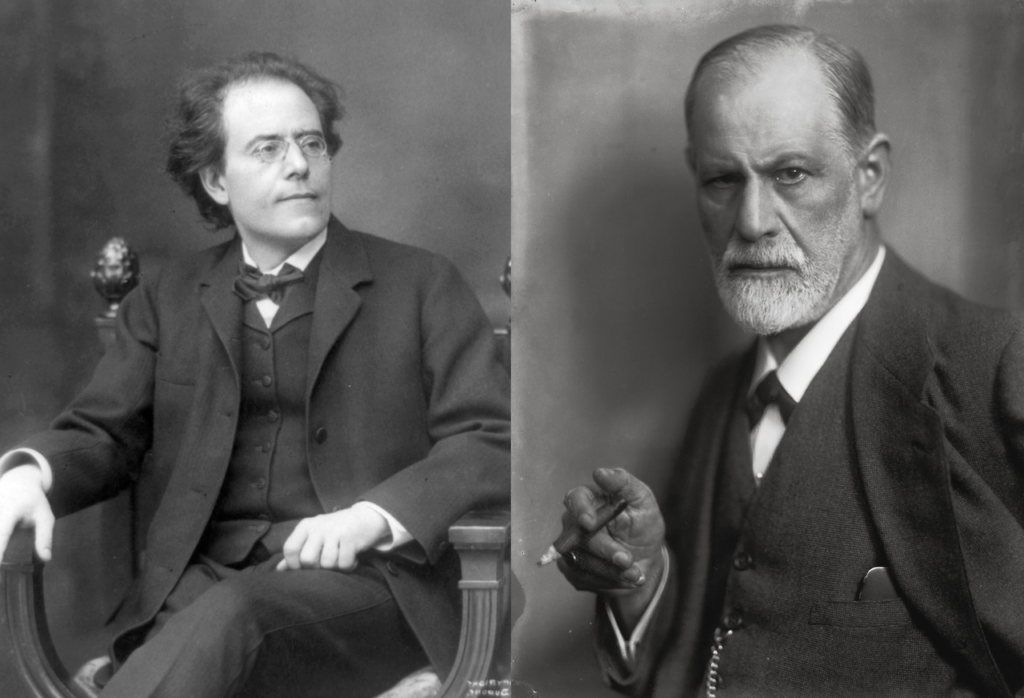
The date was August 26th, 1910. The place, Leyden, Holland — better known as the “City of Discoveries” owing to its long scientific heritage.
The people present were two giants of Viennese society, composer Gustav Mahler and psychoanalyst, Dr. Sigmund Freud.
By the time of their meeting, the method Freud had pioneered for the alleviation of mental and emotional distress was well-established. Its form was influencing clinicians around the world, best represented by the presence of a couch, free association, and years of contact carried out in frequent, but strict 50-minute “sessions.”
Mahler telegraphed Freud from Munich multiple times requesting help. The situation was dire. Mahler was “impotent,” and his wife, 19 years his junior, was deeply unhappy.
Much of what happened next is lost to history. What is known for certain is that Mahler did travel to Leyden and met with Freud, and that the composer’s sexual functioning was restored following this single meeting.
Bottom line? A great deal of good could be accomplished in a brief period of time and outside of traditional psychotherapy settings. Indeed, Freud did not meet with Mahler in an office. No couch was involved nor sacrosanct time limit. Rather, the two talked while, “strolling about the town—the stocky, confident doctor and the thin, intense composer— smoking the cigars both adored” (Sorel, 1982).
I was reminded of the foregoing story while interviewing Dr. Ed Jones for my blog and YouTube channel. Ed is a psychologist and consultant with an uncanny ability to “see around corners.” Over the years, I’ve learned to pay attention whenever he talks about trends in mental healthcare service delivery. And lately, he’s been focused on the “50-minute hour.”
“Multiple developments — including the rapid increase in the use of digital technology during the pandemic, and integration of behavioral and medical care — are challenging mental health professionals to think and act differently,” he says, then continues, “Instead of relatively circumscribed treatments episodes, delivered across multiple sessions lasting 50 minutes, therapists will need to be helpful on an ongoing, but likely intermittent basis over the course of people’s lives in interactions lasting a handful of minutes.”
Importantly, Ed does not see this development as the end of something, but rather an opportunity to expand the field’s ability to meet with, engage, and help more people in need. Let me know what you think in the comment section below.
Until next time,
Scott
Scott D. Miller, Ph.D.
Director, International Center for Clinical Excellence
P.S.: Registration for the next FIT Supervision Intensive is now open. For more information, or to register, click the link or icon below.

I began retraining in Counselling in 1999, after enjoying success as a Business Marketing & Management Consultant, and promptly opened a Private Practice in 2001, going on to complete a Double Degree and Post-Graduate study in the field.
During my study tenure, I was stunned by not only the absence of any commercial business training in Counselling but also by how many people said that they desired to be in private practice but had no idea how to run one, so they went and worked for an agency instead, some burning out and eventually leaving the sector altogether.
Part of my Practice work is coaching other therapists on how to set up a Private Practice, and/or how to grow the Private Practice they already have, without having to rely on Government or Crown Entity funding to do so.
Commercial Business Operation Management & Formal Client Outcome Measurement Tools are key components of this coaching assistance.
I’ve been booked solid for 4-6 weeks in advance in Private Practice since 2001, and have never pursued any affiliation to State funding (which I’m assuming is part of what Ed refers to as “Managed Care”).
“He who pays the piper, calls the tune” is certainly a truism in the sector, and frankly, I prefer that clients set the playlist, as opposed to a state agency.
I’m not sure if this makes me a disrupter, but I’m pretty sure I’m an iconoclast 🙂
Hi Scott
Thank you for this very interesting interview. I am great supporter of intergradting mental health services, and particulalry psychologists and counselors with the primary health care.
In 2016, I had the priviliage to be the first psychologist to start the implemntation of the program of the intergration of mental health service within PHC, as part of Hamd Medical Corporation (HMC) in the state of Qatar. Since then, the program was a success. Now the program has been introduced into many other primary health services. The hope is to break the barrier and the stigma of seeing a mental health practitioner. It also help lay people to be impowered and informed about mental health and psychotheray.
Is the “50-minute hour” done for? Great question!
I’ve long been of the opinion that the 50 minute hour is geared round the needs of practitioners and services, rather than clients. Start on the hour, provide 50 minutes, have ten minutes to write notes, start again on the hour. Maybe I’m being slightly cynical.
Now I’m in private practice, I give clients an hour. If I’m running consecutive sessions, I leave 30 minutes between them. Clients get a much better version of me that way.
Ed’s right about “ongoing, but likely intermittent basis over the course of people’s lives.” Maybe not minutes in my case, but otherwise the principle definitely applies to the way I work. It’s what many of my clients ask for.
Thanks Scott!
couldn’t have said it better myself – I give an hour, unless we don’t need it, but most do. also – I am available between sessions routinely not in crisis – most don’t use that, but some do. i have some seniors I see 2x’s week, 30 mins each. It’s whatever client and I create, w/in payment guidelines. now with virtual, it’s so much better for relationships!
while tech will always evolve what I do, I must keep boundaries, and, as a profession we must insist. I hear some of those newfangled mental health co’s are doing some disruptive things that AREN’T ethical, so, let’s go slow with this adding more tech thing. part of providing effective, efficient care IS being sure the provider doesn’t burn out.
Easy scheduling because Freud was bad with math.
Imagine surgery with “1.5h for surgery and 30 minutes after to prepare for next patient”, waking up from anesthesia in pain with stitches (and god knows what in case of orthopedic surgery) and doctor saying “we will give you some extra pain meds and see you next week”.
And it is especially important to consider that, for example, 50 to 65 minutes is not 30% longer but is effectively at least 50% longer because when “arm up” and “cool down” time is taken away 50 minutes session is hardly more than 30 minutes and adding 15 minutes is huge boost.
Often ignored is time wise efficiency for clients: it is much easier to commute once a week for a bit longer session (even if it is more expensive) that twice a week.
I find it fascinating that such basic thing is still based on tradition or even cult-like mentality. I would even dare to say, such rigid rule is more likely to hinder than facilitate real progress and that people who blindly insist on something like that with excuses like “it is about learning boundaries” are either too stupid/indoctrinated or don’t have clients’ best interests at hearts. In my experience, short sessions give constant feeling “there was not enough time” and “help” to loss therapy focus.
For me it is very unethical to insist on ineffectual or even harmful practice. I don’t care about popularity or tradition, it is not right thing. Lobotomy was popular too, blood letting and leeches have tradition of few millennia.
Hello, I have worked “integrated care” in a urban-based Federally Qualified Health Center for over 7 years. This model works! I truly thank those who went before me and trained me to “work faster” so I was prepared for this “wholesale” model of community mental health. I always wondered “Where are those other ‘diagnoses’?” [the ‘shy’ diagnoses like Avoidant P.D., OCD, GAD, etc]. Well, they all get the flu, stub their toe, need a check up: and they show up in the primary care office. I can use all my brief therapy skills AND I can do ‘intermittent’ long term therapy.
Ridiculous. Bending to the terrible model of medicine of cranking the patients through the examining room and “treating” diagnoses, rather than engaging with the human being who has come for care and whose issue may very well be a function of multiple causes, who is in distress and can benefit from compassionate attention, which can itself facilitate reduction of distress.
The future isn’t medical, according to this interview: It’s corporate. Treatment as product, done on insurance company and medical corporation imposed schedule that’s purely instrumental. It’s the auto-repair model.
One of the great benefits of therapy and the 50 minute, or longer, hour is it gives patients time and space – which few if any of us get in daily life – to experience themselves without demand that they be fixed – and find ways, in conjunction with the therapist, to make changes in how they live so they live in a way more congruent with their own sense of themselves.
Scott,
I generally concur with Jonathan. At worst, Dr. Jones’ position strikes me as yet another capitulation to the neoliberal hegemony that prioritizes corporate interests (i.e., profit) over all others. At best, his interview left me with more questions than answers. In particular, Dr. Jones makes a number of assertions without citing any evidence. A few examples:
1. Digital healthcare and digitized therapy techniques/tools “help a lot of people.”
2. Referencing “long psychotherapy sessions,” Dr. Jones asserts “that’s not going to work and people don’t want it.”
Towards the end of the interview, Dr. Jones questions what a good therapist would do in the face of this mounting corporate future. A good therapist would fight against it and encourage their colleagues to organize for the same.
A good video I’ve been working as the only fulltime medical hypnotist in New Zealand and I treat most of my cases in a maximum of 5 sessions. the sessions including the intake sessions are 90% scripted and crucially 10% individualised. GAD 7 scores at intake of 20 get reduced to 2 or less in just five sessions. The first session is crucial and I aim to raise hope and expectancy
Congratulations to Mrs. Mahler.
i love your point AND i think the field will evolve to allow both – sometimes people won’t need lots of space and time and many times they will. it will depend…as we teach clients, balance flexibility AND rigidity – w/o extremes.
yes, there is already evidence that #1 is true (there IS evidence and it’s growing every day)
having cut my therapy teeth in the 90’s when managed care was more restrictive than it is today for routine OPMH (as I can’t speak for areas I don’t practice in), the finances DO matter. there is a balance here too methinks: managed care CAN be damaging if done poorly – if done well, doesn’t micro manage.
In my opinion, this is bunk. I agree with Jonathan Levin and Sean Penny. Good therapy is based on a relationship. People get better because they are in a relationship with another human being, who provides certain psychological functions to help the client internalize and integrate what was missing or toxically present in relationships with their early caregivers. I would love to know exactly how Freud cured Mahler in one session, and what exactly what Mahler’s problem actually was. In my experience, sexual dysfunction is just a manifestation of one or more psychological issues that can take a long time to uncover and reintegrate. But anyhow, I will say that as a client it has taken almost a lifetime to uncover and process early attachment failures and a myriad of other family dynamics in my own history, many of which involved dissociated states in my caregivers and within myself. Trying to sell the public some kind of quick fixes and digital “tools” to solve complicated psychologically driven problems is a sham. There’s a place for these but abandoning the core therapist/client relationship in favor of shorter treatments and less involvement by the therapist is a disservice to potential clients. I am retired now after a 25-year career, and I am fearful of the future of our profession. I practiced psychoanalytic psychotherapy and had many successful treatments and many grateful and satisfied clients who had no interest whatsoever in coming less frequently or engaging in quick-fix types of practices.
I should have watched the video before I wrote my reply. What needs to happen is that managed care has to bend towards quality therapy of depth, insight, and relationship. It needs to accommodate to longterm practice, not the other way around.
There certainly isn’t anything magical about the 50,45 or even 60 minute mark. In a number of therapies the session time could be altered to better effectiveness.
However, to meet with a clinical struggling with i.e anxiety and offer tips in a few minutes would feel deeply unsatisfying to me as a clinician, mostly for the simply reason that tips don’t work. We know this from the research you have put out elequantly over the years. It’s not the simply technique or tip that causes change.
When therapy is successful it usually works by altering the clients inner landscape regarding whatever issues the patient is presenting with. That usually takes a bit of focus and clients receiving a tip or technique to quickly will simply adopt that into whatever problematic landscape and understanding they already hold.
I want to share a few thoughts based on these comments to my interview with Scott. I have approached these issues with two anchoring beliefs: 1) business trends are powerful socioeconomic forces to be respected, engaged and managed to the best of our ability; 2) therapy is a remarkably powerful intervention that does not scale well in its current 50-minute format, and so millions of people are being deprived of the unique interpersonal experience it provides.
Let me also respond to a few comments specifically. My goal is not to prioritize corporate interests over all else, but those interests might prevail unless our field puts its energy behind a good alternative strategy. Healthcare in the US is consolidating, and it is already about 20% of the GDP. Behavioral health companies and programs are being merged and acquired into this massive enterprise, and I worry what might happen to therapy as an institution. It will be attacked in many different ways.
My hope is that therapy can survive as it is for those needing it, and that brief visits can become normative in primary care. As Scott and others have taught us well, the impact of therapy owes more to the individual clinician than any techniques used. Let’s move those effective clinicians into a new setting to help more people than are being helped today. They are not there to “offer tips” or use evidence-based techniques, but rather to see what a brief experience of someone listening with empathy and without judgement can do. Many people are desperate for such an experience, and even a brief exposure can be the beginning of something bigger.
I am an EMDR Clinician. Sometimes those sessions don’t fit into the 50 minute box neatly. I tend to fit different phases of treatment into the allotted time. If I have 10 minutes left, I use it to connect to the client or teach grounding techniques. If we believe that processing actual trauma will take longer, we plan for longer sessions. Even using an intensive format if necessary. I do think it is necessary to think outside of the 50 minute box or else we run the risk of decreasing client care. Good points in the blog!