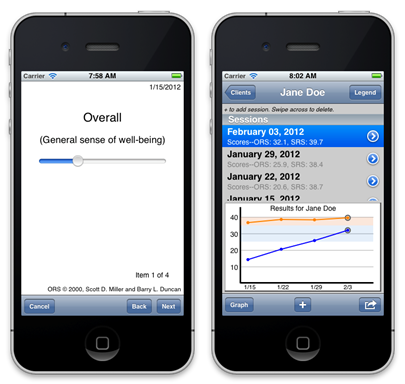
Since they were developed and tested back in the late 90’s, the Outcome and Session Rating Scales have been downloaded by practitioners more than 100,000 times! Judging by the number of cases entered into the three authorized software applications, the tools have been used inform service delivery for millions of clients seeking care for different problems in diverse treatment settings. The number of books, manuals, and “how to” videos describing how to use the tools has continued to grow dramatically.
Here is one more option for support: a recording of a live webinar discussing FIT and deliberate practice with professionals from around the world. I think you’ll be surprised by the depth and breadth of the information covered. You can listen to the entire broadcast or use the guide below to jump directly to the questions that matter most to you.
- How to get started with FIT? (2:23)
- How can I encourage my clients to provide open, honest feedback? (10:30; revisited 36:15)
- Should I start using the measures with established clients? (13:18, revisited 17:05)
- How do I know how effective I am? (14:45)
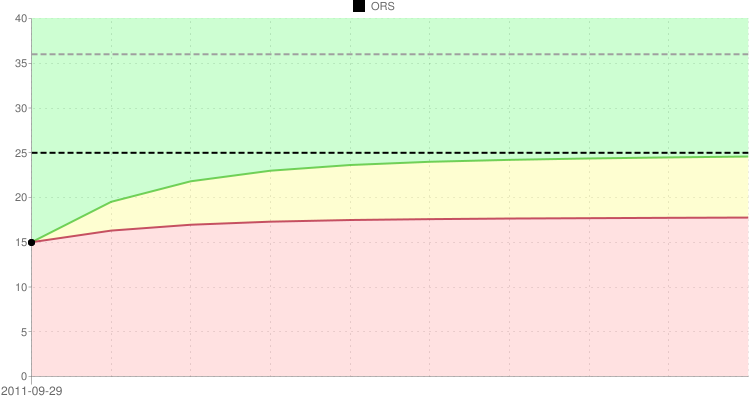
- How to interpret ORS and SRS feedback (18:10)
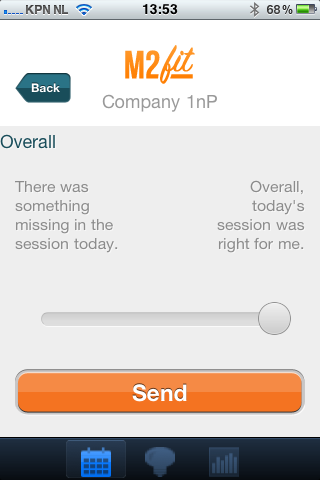
- How to use the scales online/on the phone? (22:00)
- How effective is supervision? (26:58)
- How to work with mandated clients? (31:30)
- Why do some clients not give feedback? (37:00)
- What is deliberate practice and how to apply it for improving therapist effectiveness? (46:00)






(5).jpg)