 Take a look at the graphic to the left. It shows the use of the Outcome and Session Rating Scales (ORS & SRS) from the beginning of this year to the present by users of one of the three , authorized FIT software programs.
Take a look at the graphic to the left. It shows the use of the Outcome and Session Rating Scales (ORS & SRS) from the beginning of this year to the present by users of one of the three , authorized FIT software programs.
What do you see?
A couple of things stand out for me. First, a steady rise in administrations of the tools beginning in late January and continuing to the third week of March when use significantly dropped. You can literally “see” the pandemic coming. In the weeks and months that followed, use of the measures steadily recovered and is, as of today, up nearly 30% over its record high in the weeks before virus mitigation efforts brought the world to a standstill.
The cause of the rise in online use of the ORS and SRS is no mystery. The number of therapists seeing clients virtually has, virtually, exploded. In this “brave new world” of clinical practice, its clear clinicians are looking for concrete, evidence-based ways to augment the two-dimensional sensory input (sight and sound) characteristic of video conferencing.
In a previous blog, I summarized the research on the effectiveness of online behavioral health services. The data are clear: it works. More, a brand new meta-analysis, released just this week, adds to the body of evidence documenting that being physically present is not essential for successful outcomes.
The ORS and SRS are particularly well suited for online service delivery. Indeed, the original validation studies of the two scales were actually 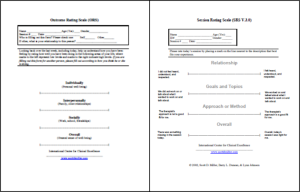 conducted in a teletherapy setting. It was the era before high-speed broadband and Zoom. Therapists spoke with their clients by landline, administering the measures orally using a standardized script. Since those early days, scores of studies have documented the impact of routinely soliciting formal client feedback on both outcome and retention in behavioral health services. In one recent study, clients of therapists using the ORS and SRS were 2.5 times more likely to experience a successful outcome. Using standardized measures as part of service delivery is now considered a “standard of care” by Joint Commission and SAMHSA. Next year, the State of California follows suit, allowing psychologists to use the tools to earn required continuing education credits (see top of page 4, under “Practice Outome Monitoring [POM]”).
conducted in a teletherapy setting. It was the era before high-speed broadband and Zoom. Therapists spoke with their clients by landline, administering the measures orally using a standardized script. Since those early days, scores of studies have documented the impact of routinely soliciting formal client feedback on both outcome and retention in behavioral health services. In one recent study, clients of therapists using the ORS and SRS were 2.5 times more likely to experience a successful outcome. Using standardized measures as part of service delivery is now considered a “standard of care” by Joint Commission and SAMHSA. Next year, the State of California follows suit, allowing psychologists to use the tools to earn required continuing education credits (see top of page 4, under “Practice Outome Monitoring [POM]”).
If you don’t have copies, you can get them for free here. Looking for detailed instructions and “how to” videos on integrating the ORS and SRS into online services, click here — all free.


