 Eighty three million, six hundred fifty thousand, thirty seven.
Eighty three million, six hundred fifty thousand, thirty seven.
Can you guess what this number represents?
No, its not the net worth of the latest tech millionaire. Neither is it the budget of a soon-to-be released Hollywood blockbuster.
Guess again.
Give up?
It’s the number of adults in the U.S. who reported struggling with mental health or substance use resulting from efforts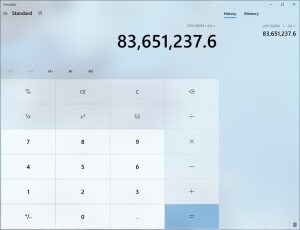 to mitigate the SARS-COV-2 virus.
to mitigate the SARS-COV-2 virus.
By the way, that figure is from the last week in June, three months ago. Since then, the isolation, job losses, and economic and political uncertainty and social unrest have continued.
According to the Center for Disease Control, “Younger adults, racial/ethnic minorities, essential workers, and unpaid adult caregivers reported having experienced disproportionately worse mental health outcomes, increased substance use, and elevated suicidal ideation,” with a staggering 25% of 18-24 year-olds having seriously contemplated suicide in the weeks prior to completing the survey.
One glimmer of hope amidst these dire statistics is that access to mental health care has expanded during the pandemic. In March, U.S. government agencies expanded Medicaid telehealth coverage. In turn, the U.S. Department of Health and Human Services relaxed HIPPA privacy rules, further reducing barriers to accessing treatment remotely. Many third party payers have followed suit. As it is, the dramatic increase in those seeking mental health care and shift to virtual service delivery fit squarely with the theme of this year’s World Mental Health Day. Falling on Saturday, October 10th, it calls for “ensur[ing] that everyone, everywhere has access to mental health care.”
 Of course, increased demand and easier access to care are placing a strain on therapists. As one recent story noted, “Therapists and counselors are facing the same anxiety, uncertainty and financial stress that are troubling those who seek their services.” The risk of a “parallel pandemic” of burnout is, according to recent studies, rising. Consider this, prior to the outbreak, available evidence indicated between 21 and 67 percent already were experiencing high levels.
Of course, increased demand and easier access to care are placing a strain on therapists. As one recent story noted, “Therapists and counselors are facing the same anxiety, uncertainty and financial stress that are troubling those who seek their services.” The risk of a “parallel pandemic” of burnout is, according to recent studies, rising. Consider this, prior to the outbreak, available evidence indicated between 21 and 67 percent already were experiencing high levels.
Not long ago, my colleague Mark Hubble and I reviewed the research on the subject noting that most of currently fashionable approaches (e.g., practice mindfulness meditation, eat healthy snacks, go for short walks, exercise regularly, get enough sleep, join a service organization, take up a hobby, attend a continuing education event, learn to say no, see a therapist, and take time out to value oneself) not only don’t work but often make matters worse.
What does work?
I hope you’ll read (or re-read) the article. It’s free and provides a detailed review. That said, all things being equal, one key finding is that effectiveness mitigates risk. Said another way, the better a therapist’s results, the less likely they are to burnout. The challenge, particularly in these troubled times, is that we care. People matter to us. We want to make a difference. In this effort, we place ourselves at risk whenever what we’re there to accomplish takes a back seat to the caring, empathy, and compassion we provide, no matter how lovingly extended.
Bottom line: keep outcome front and center in your work. After all, genuinely and demonstrably helping people improve is the entire point of therapy and, in the end, the best of all ways to show that we really, deeply care. One way to do that, of course, is to measure your results. If you haven’t already done so, you can get my two, evidence-based progress and relationship scales for free by clicking here. If you need some help learning how to integrate the tools into your online work, check out the many blogposts, how-to videos, and webinars my colleagues and I have produced since the start of the outbreak (1, 2, 3, 4)– again, all free.
If you are looking for a way to improve your effectiveness, my colleague and co-author, Daryl Chow, are launching a self-paced, e-learning workshop on deliberate practice, based on our new book, Better Results. Beginning November 2nd, we’ll start what we call the “DP Drip.” Every Monday and Friday for nearly three months, you’ll receive links to brief videos and other goodies aimed at helping you design and execute your own deliberate practice plan. To ensure you get the individualized help you need, its limited to 40 participants. Interested? Click here to watch a short, introductory video.
OK, that’s it for now.
Scott
Scott D. Miller, Ph.D.
Director, International Center for Clinical Excellence


Leave a Reply