So, how much time do you spend doing paperwork? Assessments, progress notes, treatment plans, billing, updates, etc.–the lot?
When I asked the director of the agency I was working at last week, it took him no time to respond. “Fifty percent,” he said, then added without the slightest bit of irony, “It’s a clinic-wide goal, keeping it to 50% of work time.”
Truth is, it’s not the first time I’ve heard this figure. Wherever I travel–whether in the U.S. or abroad–practitioners are spending more and more time “feeding the bureaucratic beast.” Each state or federal agency, regulatory body, and payer wants a form of some kind. Unchecked, regulation has lost touch with reality.
Just a few short years ago, the figure commonly cited was 30%. In the last edition of The Heart and Soul of Change, published in 2009, we pointed out that in one state, “The forms needed to obtain a marriage certificate, buy a new home, lease an automobile, apply for a passport, open a bank account, and die of natural causes were assembled … altogether weighed 1.4 ounces. By contrast, the paperwork required for enrolling a single mother in counseling to talk about difficulties her child was experiencing at school came in at 1.25 pounds” (p. 300).
Research shows that a high documentation to clinical service ratio leads to higher rates of:
- Burnout and job dissatisfaction among clinical staff;
- Fewer scheduled treatment appointments;
- No shows, cancellations, and disengagement among consumers.
Some potential solutions have emerged. “Concurrent ,” a.k.a., “collaborative documentation.” It’s a great idea: completing assessments, treatment plans, and progress notes together with clients during rather than after the session. We started doing this to improve transparency and engagement at the Brief Family Therapy Center in Milwaukee, Wisconsin back in the late 1980’s. At the same time, it’s chief benefit to date seems to be that it saves time on documentation–as though filling out paperwork is an end in and of itself!
Ostensibly, the goal of paperwork and oversight procedures is to improve accountability. In these evidence-based times, that leads me to say, “show me the data.” Consider the wide-spread practice–mandate, in most instances–of treatment planning. Simply put, it is less science than science fiction. Perhaps this practice improves outcomes in a galaxy far, far away but on planet Earth, supporting evidence is spare to non-existent. Where is the evidence that any of the other documentation improves accountability, benefits consumers, or results in better outcomes?
Put bluntly, the field needs an alternative. What practice not only insures accountability but simultaneously improves the quality and outcome of behavioral health services? Routinely and formally seeking feedback from consumers about how they are treated and their progress.
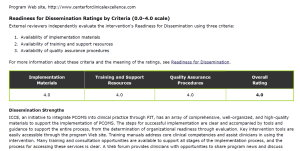
Soliciting feedback need not be time consuming nor difficult. In 2013, two brief, easy-to-use scales were deemed “evidence-based” by the Substance Abuse and Mental Health Services Administration (SAMHSA). The International Center for Clinical Excellence received perfect scores for the materials, training, and quality assurance procedures it makes available for implementing the measures into routine clinical practice:
Then again, these two forms add to the paperwork already burdening clinicians. The main difference? Unlike everything else, numerous RCT’s document that using these forms increases effectiveness and efficiency while decreasing both cost and risk of deterioration.

First time in my life have not been able to contain work.
Am in private practice.
Am starting seriously to think through how to re-arrange.
I love the article, I am a therapist in Florida and in all honesty. I can’t stand Medicaid at all. I say at least for me working in clinics the paperwork is more 75% of my time. It’s really stinks when the time should be focused on clients. Stats in mental health is rising, I wonder why? Something needs to be done on National level to cut down the tedious, ridiculous paper. I never understood why a bio for a 5 year child needs to be 15 pages or repetive questions.
Take a look at page 4 of the above-referenced document for details regarding how paperwork is handled at local walk in clinics.
http://www.brieftherapynetwork.com/documents/Walk-in.pdf
Hi Scott,
Yes, I definitely spend more time on paperwork than 5 years ago and yes, it definitely takes time away from work with my clients.
I am clinical supervisor of 6 clinicians in CYMH clinic and for all of us I can definitely say TOO MUCH
Thank you for raising this isse.
I work in a correctional institution. More than 75% of my time is spent on paperwork. Some of my coworkers disagree with me. They believe the actual number is closer to 85%, and I am not surprised. One reasons, in my opinion, for this high level of waste on “clinical” hours is that the state agency I work for is being monitored for compliance with the court orders to provide care to the mentally ill offenders at various levels. There is no need for the actual care and there’s no accountability for the quality of care. Although I am a very computer-savvy clinician and can utilize technology to maximize my face-to-face contact with the patients, I am forced to do a lot of paperwork. Regretfully, the agency is using the technology to create more paperwork. Alas! The agency utilizes computers to create neat forms and requires clinicians to type their notes, etc. and awkwardly considers this an efficient use of technology. I want o scream…
Thank you for your excellent article!!
I am a Mental Health Therapist who was recently hired at a counseling center. I can relate to most of the comments. So far it seems like they cram as many clients as you can in one day, but then expect soooooo much paperwork to be done by each client, that there aren’t encough hours in the day to do it all! Realistically to properly get the amount of paperwork they want done, it would take an hour per client. There are not enough hours in the day! So what happens is, you come in early and stay late (Im on salary) and still not get it all done!!! There are very few people who have worked there more than a year!!!! The burnout and turn over rate is sooo High! (of course, I didn’t know when I got hired). I am praying to just get through my first 90 days! Help!
Too Much.
We’re not alone in this – see “The Atlantic” Nov14 “Doctors Tell All” – a review of books by disillusioned physicians showing that the problem is becoming ubiquitous.
Way too much! 50% is for routine documentation. That percentage increases with unusual requests or circumstances. That combined with declining reimbursement is making private practice almost impossible. I work much longer hours today, seeing approximately the same number of patients and doing the same kind of work that I did 10 to 20 years ago but getting paid less. And work under the constant threat of insurance audits that require people to repay monies earned for services already provided.
Too much by a long shot.
The staff at my workplace are required to meet productivity levels that make it impossible to complete the notes during normal work hours. Thus, we work during our personal time on evenings and weekends in order to complete progress notes and intakes, in addition to working on notes during the work day. Staff believe that our detailed, 2-3 page progress notes are required by the Joint Commission. I have not heard of any complaints by the Joint Commission about our notes, so I wonder if that’s accurate or if it’s lawyers being overly cautious. We have had additional paperwork added to our task list, all of it well-intentioned and meaningful, but there has been no commensurate reduction in productivity requirements, so these added documents will require greater use of personal time to complete. For professionals who promote the mental health of clients, you’d think we’d look after our own mental health, too.
Although it goes against my ethics of wishing to serve those in need, I recently had to stop accepting Medicaid patients in my private practice because of the amount of behavioral mumbo jumbo required in their treatment plans and the frequency of need to write another plan to request additional services. The details requested have no relation to factors that determine effective treatment and as a psychologist with a spinal cord injury and limited time available to see clients, I’ve had to turn my back on these clients.
I first met you when you started working with Insoo and Steve in Milwaukee ,Wisconsin. I was doing some work with them in New Mexico..
In reference to your question, it is obvious that paperwork has increased only it’s now on the computer and the clinician does all their own paperwork. intake assessments are required before any counseling which includes a two hour block requiring that the treatment plan B completed the same time. There is no or little time involved in rapport building the families or even getting to know the client through developing therapeutic rapport. I sincerely hope we can join together to address legislative sessions throughout the country as prevent the demise of mental health therapeutic rapport replaced by a business model
far too much paperwork. Bevan & Hood (2006) is the paper to read on ‘targets and terror’ and ‘gaming’ of health statistics – the form of management that crashed the Soviet economy – where there is now a whole industry of health target measurers where people cook the statistics for them, and they don’t check because if they are getting the figures they want they are happy. This industry deliberately excludes FIT – see for example Sasiak et al (2012) Measuring outcome in child and adolescent mental health services: …’ Clinical Child Psychology and Psychiatry, 18, 4: 519-535. (A NZ study – no mention of FITS despite now in use in numerous hospitals).
Yes the amount of paperwork has increased. In my opinion, some of the forms are just not well designed and the same i formations is repeated in several forms inside the same file. I believe that several forms could be combined into one easily.
I work for the federal government and for every 30 mins of direct patient contact I am spending 30 mins to document that encounter that includes all the risk assessments and SOAP notes that I am mandated to complete. Talk about redundancy I also have to literally document all of this into two separate military records systems. I am forced to make the choice between providing “world class” (which is in the mission statement) patient care versus closing out records to meet unrealistic demands. Of course I choose to provide my patients with “world-class” care, that is why I choose to work with the military, and therefore face being perceived by my superiors as not being effective with “time management”. Rediculous !!!!
Yes, I am spending more time on paperwork and than I was 5 years ago. Usually 30%, and sometimes 40%.
It isn’t taking time away from my work with clients, it’s help me in my work with my clients.
Best regards,
Doina
Too much paperwork!
Absolutely too much!
Far too much in the State of MN!!!!
We do too much paperwork. A vast portion of it is to justify our existence ie. for contractual obligations to the government, not for client care. The rationale is not justified. Less paperwork obligations and more opportunities for direct client care would be optimal.
Yes paperwork has increased, and it depends on who you are serving just how extensive it is. They range from the legal/ethical license requirements to the insurance carrier that is data intensive. My biggest complaint is that the paperwork requires the clinician to think in terms of case development in the way the paperwork requires it, which sometimes is not a match.
My answer to your question is to say that as a private practitioner in the UK I still have a very light paperwork load. Long may it continue – but the forces of darkness are spreading. National registration is coming.
On another note, you might enjoy this – my homage to you Scott.
In my NHS practice there is alot of extra documentation I need to check is complete prior to inspection by the Care Quality Commission (CQC). This important government agency are focused on what documentation looks like rather than quality of improved experience for patients. I will have to allocate about one week in which I am not seeing patients.
I think the culture associated with documentation can make some clinicians aversive to risk and less likely to take on work. I tend to take on more as the risk averse clinician takes on less. I had been advised to find ways to offload or pass work to someone else. I feel I unable to do this in our small team.
To find the delicate balance of paper justification to satisfy federal, state, and insurance providers and actually do therapy is an exercise in patience.
Having worked in community behavioral health the load is enormous…
Now in a private setting I’m loving doing therapy again and using spoken dictation technology to assist in my documentation.
I have heard many arguments for concurrent documentation and I believe there is power in presence, focus, eye contact, and human connection….all of those subtle gifts seem diminished when a piece of hardware is included in the therapeutic relationship.
I absolutely spend more time in the electronic medical record world on documentation. I work at a local mental health center that no longer has maintained full time salaried positions in the outpatient program. We are all now FFS employees and have been moved to the 45 minute block where we see more people in a day and are expected to do “concurrent billing” It is daunting to clients to complete the “hoops” for such needs as JCAHO accreditation and insurance standards and feel that they have gotten their copayment’s worth of “talk time.” . Many, many clinicians leave to enter private practice and we have have fewer and fewer staff with clients feeling the abandonment issue with each departure.
Hello Scott.
Too much!
Working as a clinical psychologist in public health care in Norway, we have at present a national debate regarding the amount of paperwork in the field. In focusing on the clinical staff, and the time consuming documentation routines, leaving less time to direct clinical work, I have introduced the term “non- completion fatigue” to describe the possible negative consequences for staff members/ clinical workers that almost never get the time or feedback to perform “good” enough work…..
AndersD, ph.d
Scott,
Paper is our client in many setting that I consult and in my own experience in the public sector. We did two time studies, one in last 1999 with 17 clinicians and determined that, at that time, the ave. for typical documentation was 27 percent of the clinician’s time. This did not include meetings and sundry other ‘demands’ on the their time. The last official look was in 2008 at a large community mental health facility. With 20 professionals doing a time-study, the time spent was 32 percent on routine paper work. This was also using a state mandated on-line computer program. An interesting insight was that although the bulk of the documentation was upfront, a significant portion was trying to continue authorization with Medicaid and QA folks within the state.
More anecdotally, in numerous agencies where I have clinically consulted, the numbers typically cited are a third of their time. This has launched a lot of concurrent documentation schemes and processes. Finally, I believe that much of the documentation quality (meaningfulness, accuracy, conceptualization, and insightfulness) has been eroded by the demand for quantity and fixed data points. With this in mind, it is not surprising that most clinicians that I work with and know are working between 47- 52 hours weekly and being paid for forty because of productivity quotients and demands…………
Scott,
I am so busy that I can’t take time to do this properly! This speaks volumes. I work in the schools and there is so much paperwork for special education that it certainly impinges upon not only my job as a licensed school psychologist but special education teachers as well. I have known many a early special educators with master’s degrees working 12 to 14 hour days plus weekends to get the paperwork completed. Many whom don’t have families or are married! Having said that, many are looking to exit this field by getting into a doctorate programing and looking to become college/university professors. Little do they know that most of the time only adjuncts are hired!
Be well and Happy Thanksgiving!
Bill Hosmer, Ph.D.
Hello Scott,
I work for a CMHC in Washington state. The agency has introduced concurrent documentation for the clinician’s due to several factors. One is the mandate from the state to get 1080 face to face hours per month. Another is the mandate to have all notes done within 72 hours. Another one is the extraordinary amount of paperwork that needs to be done in a timely manner. I was hoping that with the advent of our E.H.R. that paperwork would be reduced. However, when we had paper charts you had to do one form to reauthorize a client for additional services. Now not only do you have to complete that form but you also have to do three other online forms for the process. So one form turned into four forms! TOO MUCH!
Hello Scott!
I am still doing clinical work, group-, family- and individual therapy. And a lot of supervision. And I enjoy doing that! (At the age of 69.) The Norwegian government demand me to report how many patients, diagnoses, hours and so forth, three times every year and that has gone from once a year to three times a year! But when it comes to the rest of the paperwork, it is more or less the same as five years ago! So thats all. I am now in France, and write you more personal when I return to my computer in Norway.
Peter Rongved
Sendt fra min iphone
I am in private practice. I quit being on insurance panels because of paper work and now things are fine. I do not do workmans comp either for that reason. I bill for patients and keep my notes and that is about it. I do ask your scaling questions almost every session and find them very helpful but I do not document them.
Good evening,
for me, in the past 5 years ago I was working only in private practice and I have no rapports to make for statal agency, so
· I’m not spending more time on paperwork than the last place of work, 6 years ago
· I’m not taking time away from my work with my clients.
Best regards,
Dr. Josephina NEAGU-SLOBOZEANU
PsyMotion – Clinica de psihiatrie, psihoterapie si dezvoltare personala
Str. Mihail Sebastian, nr. 203, sect. 5, Bucuresti
Tel./Fax: 021.781.22.59
From: Reg Reynolds
Date: Mon, Nov 24, 2014 at 10:34 AM
Subject: Re: Can I ask your opinion?
To: enda.madden@acehealth.co
Reg Reynolds
I am in independent practice, so I can’t answer your question directly. However, I used to manage a psychology department and, when the institution that I worked for demanded that the psychology staff sign in and out, the hours that they put in dropped from 54 per week to slightly under 36 per week. 🙂
40-50% of time spent on paperwork!
I have seen the reimbursement rates remain the same -or lower, during the past sixteen years. Concurrently, the time spent -even in private practice, involving billing, collecting, and keeping up to date with required changes (HIPPA, new 2013 CPT codes, etc.), has significantly increased.
The above is only the case of Commercial Insurance Companies. If we include Federal Programs in the conversation, such as Medicaid, the numbers are much worse. Those reimbursement rates have decreased to an insulting level for any professional with Master’s degree or higher, and the paperwork has tripled!
As a private practitioner, it has pained me to arrive at the decision of not accepting Medicaid assignments. However, the alternative would have been closing the doors soon after due to the practice becoming financially unsustainable.
The end result? Private practices with much fewer clients, and people with limited resources not receiving needed services….
Paperwork is more demanding now than 5 years ago. About 7 years ago is was even better (paper files).
It is taking time away that I used to spend on client contact.
The tail IS wagging the dog!!!!! Way too much paperwork simply to CYA!
Throughout my 20 year career as a child and adolescent therapis I have seen the productivity and documentation demands increase to the extent that it is now standard practice for an outpatient therapist to see over 34 patients a week while an access worker will perform 28 initial or diagnostic evaluations per week. Salaries have not gone up accordingly, documentation standards are more stringent, and a therapists worth (whether you stay or are fired) depends not on patient satisfaction and positive outcome measures but solely on documentation. This is a sorry state of affairs as I know many “iffy” therapists who receive glowing scores.
As someone relatively new to the field, and with extensive experience in quality and efficiency in other contexts, I have very quickly become disillusioned and burned out. The client experience and clinical skills receive little emphasis or appreciation. I long to interact with professionals who emphasize and value clinical skills over paper pushing.
I feel exactly the same
It stems from managed care – which itself has become obsessed with profits and is filled with incompetence. Managed care is destroying the entire economy on a grand scale and wrecking all healthcare fields that use it in any way.
If it is Erik, then MC is in a Folie a Deux with the professional organizations, especially the two APA’s. In the press releases, building a better relationship with them was a chief objective of the committee.
Well I know this is old but I just walked out of a psychologists office because she handed me about 35 forms to fill out. I have chronic pain and the injury I sustaining happened in 1989. I am having a internal stimulator put in next week and the doc asked if I wanted to sit down and talk to someone? I said sure why not. 30 years of history on my injury? I would have been there filling paperwork out for a year. I thanked her and walked out. So, question to you docs, aside from the court-ordered referrals, how do you get any patients? No way am I filling all this out. I just wanted someone to TALK to. If I wanted to write my memoirs over the last 30 years, I would do just that. Crazy!