 Last week, I was preparing to leave the house and could not locate my keys. Trust me when I say, it’s embarrassing to admit this is not an infrequent occurrence.
Last week, I was preparing to leave the house and could not locate my keys. Trust me when I say, it’s embarrassing to admit this is not an infrequent occurrence.
Logic and reason are always my first problem solving choices. That’s why I paused after looking in the kitchen drawer where I am supposed to keep them, along with my wallet and glasses, and found it empty. When did I last have them? Not finding them there, the “search” began.
Upstairs to the bedroom to check my pants pockets. No. Downstairs to the front closet to look in my coat. No. Back upstairs to the hamper in the laundry room. No. Once more, down the stairs to the kitchen hutch. I sometimes leave them there. This time, however, no. I then headed back up the stairs to the master bathroom — my pace now a bit frantic — and rummaged through my clothing. No. They’ve gotta be on my office desk. Down two flights of stairs to the basement. Not there either.
In a fit of pique, I stormed over to the landing, and yelled at the top of my voice, “DID SOMEONE TAKE MY KEYS?” the accusation barely concealed. Although my head knew this was nuts, my heart was certain it was true. They’ve hidden them!
“No,” my family members kindly reply, then ask, “Have you lost them again?”
“Arrgh,” I mutter under my breath. And that’s when I do something that, in hindsight, make no sense. I wonder if you do the same? 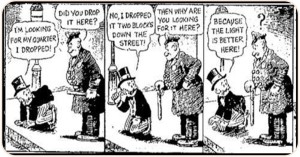 Namely, I start the entire search over from the beginning — pants, coat, hamper, closet, hutch, office — often completing the exact same cycle several times. Pants, coat, hamper, closet, hutch, office. Pants, coat, hamper, closet, hutch, office. Pants, coat, hamper, closet, hutch, office.
Namely, I start the entire search over from the beginning — pants, coat, hamper, closet, hutch, office — often completing the exact same cycle several times. Pants, coat, hamper, closet, hutch, office. Pants, coat, hamper, closet, hutch, office. Pants, coat, hamper, closet, hutch, office.
I can’t explain the compulsion, other than, by this point, I’ve generally lost my mind. More, I can’t think of anything else do. My problem: I have somewhere to go! The solution: Keep looking (and it goes without saying, of course, in the same places).
(I did eventually locate my keys. More on that in a moment)
Yesterday, I was reminded of my experience while reading a newly released study on the treatment of trauma. Bear with me as I explain. Over a decade ago, I blogged about the U.S. Veteran’s Administration spending $25,000,000 aimed at “discover[ing] the best treatments for PTSD” despite a virtual mountain of evidence showing no difference in outcome between various therapy approaches.
Since that original post, the evidence documenting equivalence between competing methods has only increased (1, 2). The data are absolutely clear. Meta-analyses of studies in which two or more approaches intended to be therapeutic are directly compared, consistently find no difference in outcome between methods – importantly, whether the treatments are designated “trauma-focused” or not. More, other highly specialized studies – known as dismantling research – fail to provide any evidence for the belief that specialized treatments contain ingredients specifically remedial to the diagnosis! And yes, that includes the ingredient most believe essential to therapeutic success in the treatment of PTSD; namely, exposure (1, 2).
The new study confirms and extends such findings. Briefly, using data drawn from 39 V.A. treatment centers, researchers examined the relationship between outcome and the degree of adoption of two so-called “evidence-based,” trauma-informed psychotherapy approaches — prolonged exposure and cognitive processing therapy. If method mattered, of course, then a greater degree of adoption would be associated with better results. It was not. As the authors of the study conclude, “programs that used prolonged exposure and cognitive processing therapy with most or all patients did not see greater reductions in PTSD or depression symptoms or alcohol use, compared with programs that did not use these evidence-based psychotherapies.”
So what happens now? If history, and my own behavior whenever I lose my keys, is any indication, we’ll start the process of looking all over again. Instead of accepting the key is not where we’ve been looking, the field will continue it’s search. After all, we have somewhere to go — and right back to the search for the next method, model, or treatment approach, we go.
It’s worse than that, actually, as looking over and again in the same place, keeps us from looking elsewhere. That’s how I generally find my keys. As simple and perhaps dumb as it sounds, I find them someplace I had not looked.
And where is the field not looking? As Norcross and Wampold point out in an article published this week, “relationships and responsiveness” are the key ingredients in successful psychological care for people who are suffering as a result of traumatic experiences, going on to say that the emphasis on model or method is actually harmful, as it “squanders a vital opportunity to identify what actually heals.”
Improving our ability to connect with and respond effectively to the diverse people we meet in therapy is the focus on Deliberate Practice Intensive, held this August in Chicago, Illinois. Unlike training in protocol-driven treatments, studies to date show learning the skills taught at the workshop result in steady improvements in clinicians’ facilitative interpersonal skills and outcomes commensurate with the rate of improvement seen in elite athletes. For more information or to register, click here.
Until next time,
Scott
Scott D. Miller, Ph.D.
International Center for Clinical Excellence




You are a great communicator. Thanks for the update. We are swamped with Trauma Based Treatment ideas and everybody is tweeting, faceboooking, and suggesting we read Vander Kolk! I have and it essentially tells me to get another Doctorate because I am a stupid old guy that still tries to relate to people and listen carefully.
The warnings about doing more harm if we fail to get people’s eyes to flutter or don’t do YOGA with them.
Thanks for reinforcing my ideas and disabusing me of the abuse and trauma I received from the experts.
Will you EVER come to the Northwest????? Specifically, Boise, Idaho. Yes, really.
Scott and Colleagues
When I read some of the research on trauma I am reminded of the 5 Financial Newsletters I receive. These are most of top rated financial newsletters in the field and the writers are very experienced, very competent and very knowledgeable in their field. The massive data, graphs and tables etc, they have access to online is the same. Still they are very selective in what they report as they see things through very different lenses. So their interpretations of the financial data differs greatly and their recommendations are frequently quite different from each other. In there own way they are not just informing and educating but also trying to persuade the reader (me and others)) This is OK with me as I sort through these reports and integrate them in my own way. Then I decide what to do.
In the psychotherapy field it appears to be very similar. Same data available but different lenses and interpretations and attempts at persuasion. As long as it doesn’t get ‘political’ and involve attacks on other points of view I am OK with it. For example.
It is always good to go back to the original references.
Norcross and Wampold reference a number of meta-analysis of trauma based treatments.
The most recent is the 2016 meta analysis called:
The relative efficacy of bona fide psychotherapies for post-traumatic stress disorder: a meta-analytical evaluation of randomized controlled trials (2016)
by Ulrich S. Tran and Bettina Gregor
(BTW the so-called bona fide psychotherapies don’t include the more recent somatic therapies such as Sensorimotor Therapy,
Somatic Experiencing; Emotional Freedom Techniques and
Accelerated Resolution Therapy among others)
Reading the article online this morning I discovered that in fact prolonged exposure and exposure therapies did slightly outperform other approaches and specific trauma based therapies did outperform non specific trauma based therapies though again slightly compared for example to supportive, present-centered, problem-solving, and psycho-educative element oriented therapies.
This is not to say that “The therapeutic relationship and responsiveness/treatment adaptations don’t rightfully occupy a prominent, evidence-based place in any guidelines for the psychological treatment of trauma.” However it is not the whole picture.
Note that trauma focused therapies and exposure focused therapies did in fact come out ahead in the meta-analysis.
See below
BMC Psychiatry. 2016; 16: 266.
Published online 2016 Jul 26. doi: 10.1186/s12888-016-0979-2PMCID: PMC4962479PMID: 27460057
The relative efficacy of bona fide psychotherapies for post-traumatic stress disorder: a meta-analytical evaluation of randomized controlled trials (2016)
by Ulrich S. Tran and Bettina Gregor
Here are parts of their results, conclusions and description of types of treatments.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4962479/#
Results
Head-to-head comparison between trauma focused and non-trauma focused treatments revealed a small relative advantage for trauma focused treatments at post-treatment (Hedges’ g = 0.14) and at two follow-ups (g = 0.17, g = 0.23) regarding PTSD symptom severity. Controlling and adjusting for influential studies and publication bias, prolonged exposure and exposure therapies (g = 0.19) were slightly more efficacious than other therapies regarding PTSD symptom severity at post-treatment; prolonged exposure had also higher recovery rates (RR = 1.26). Present-centered therapies were slightly less efficacious regarding symptom severity at post-treatment (g = −0.20) and at follow-up (g = −0.17), but equally efficacious as available comparison treatments with regards to secondary outcomes. The improved omnibus test confirmed overall effect size heterogeneity.
Conclusions
Trauma focused treatments, prolonged exposure and exposure therapies were slightly more efficacious than other therapies in the treatment of PTSD. However, treatment differences were at most small and far below proposed thresholds of clinically meaningful differences. Previous null findings may have stemmed from not clearly differentiating primary and secondary outcomes, but also from a specific use of the omnibus test of overall effect size heterogeneity that appears to be prone to error. However, more high-quality studies using ITT analyses are still needed to draw firm conclusions. Moreover, the PTSD treatment field may need to move beyond a focus primarily on efficacy so as to address other important issues such as public health issues and the requirements of highly vulnerable populations.
*******
Types of Treatment
Types of treatment included in the analyses were: Exposure therapies (EX), prolonged exposure (PE [42]), and both combined (EXPE), EMDR [41], cognitive behavioural therapies (CBT), and present-centered therapies (PCT). PCT included bona fide psychotherapies that were mostly linked to elements of Roger’s client-centered psychotherapy [43] and encompassed supportive, present-centered, problemsolving, and psychoeducative elements. Treatments coded as CBT included some therapies that utilized, but did not primarily rely on, elements of other therapies (e.g., exposure [44, 45]), and treatments such as Seeking Safety [46] or Image Rehearsal [47].
All treatments were coded whether they were trauma focused (TF) or not (NTF). TF treatments were defined as focusing on the memory for the traumatic event and/or on trauma-related appraisals [12]. Najavits and Hien [48] recommended to name non-trauma focused therapies for what they are providing and not just to qualify them for what they are not providing. Nevertheless, we adhered to TF/NTF distinction as it is frequently used in this field of research. The TF/NTF distinction served to strictly compare two categories on the same level of abstraction and to address the question of whether trauma focused treatments were more efficacious than non-trauma focused ones. Again, treatment descriptions in studies were utilized as closely as possible to code whether treatments were trauma focused or not. Within the CBT category we also examined the efficacy specifically of trauma focused treatments that included elements of exposure (TFCBT + EX).
Many Blessings for Peace and Happiness
Phil
Hi Scott,
Firstly, congratulations on breaking the cycle that allowed you to find the keys.
Secondly, congratulations on writing such beautiful lines. Loved reading the whole story, and thirdly, where did you find the keys? What led you to look elsewhere.
Most importantly, how can others learn to slightly be more creative when looking for treatment solutions – instead of boringly (and harmfully as you alluded to in your writing..) repeating the cycle.
Interestingly, I was writing an essay (for psych major)…and surprise surprise, I actually found exactly what you were alluding to, to also be found in so many cognitive psych articles. But what do I know.
Thanks again. I hope you have a moment to read this. I really like what you write.
2 coAngel’s. The first:
Only One Shoe
by John Forster & Tom Chapin
© 2005 Limousine Music Co. & The Last Music Co. (ASCAP)
Mommy, oh Mommy, what can I do?
I want to go out and I can’t find my shoe!
Did you look in the closet? I didn’t. Well, do!
You’re not going out with only one shoe!
I’m here in the closet, it doesn’t look good,
One cross-country ski and your coat with a hood,
There’s jackets and racquets, a bottle of glue.
But Mommy, oh Mommy, I can’t find my shoe!
Did you look in the basement? I didn’t. Well, do!
You’re not going out with only one shoe!
I’m here in the basement. It’s dark and it’s damp.
A barbell, some lumber, an old skateboard ramp,
There’s hammers and chisels and screwdrivers too.
Lots of great stuff, Mom, but so far no shoe.
Did you look in the attic? No. Well, hurry, tout de suite!
You’re not going out without shoes on your feet!
I’m up in the attic. There’s some kind of nest,
Cobwebs and droppings, a dusty old chest,
And photos of Grandma and Grandpa and you.
Piles of clothes, but no trace of my shoe.
Oh me, what can I do? I haven’t got a clue.
It’s really discouraging, maddening too.
Where, oh where is my/your shoe?
Did you look in the living room? Look in the hall?
Look in the bathroom? I looked in them all!
Did you look everywhere? That’s what I said!
How ’bout your room? Under your bed?
I’m here in my room, under my bed.
There’s a beach ball, a snowsuit, an old bobble-head.
A few Reese’s Pieces, a stuffed kangaroo,
And Mommy, oh Mommy, I just found my shoe!
Isn’t it funny,
Whenever we lose a toy or a shoe or a book.
Though we turn every room in the house inside out,
It’s always the last place we look!
This song appears on Tom Chapin’s Some Assembly Required CD.
Return to Home Page
Send comments to info@tomchapin.com
© 1997 – 2015 Sundance Music Inc.
100 Cedar Street, Suite # B-19, Dobbs Ferry, NY 10522 (914) 674-0247
Second comment:
Regarding work on PTSD, if you work with veterans, it is worth your time to look up Betty Merritt at the Merritt Center in Payson Arizona. She pairs senior returned veterans with newly returned veterans in a for weekend program, free to the veterans paid for by donations. This is not a commercial for her program, but an invitation to research.
Best regards to all who do this work, the work of angels.
Fascinating thoughts! Thanks so much for writing/sharing…..