 The last two years have been difficult. Whether through illness, death of loved ones, job loss, economic insecurity, or social isolation, few have escaped the consequences of the worldwide pandemic.
The last two years have been difficult. Whether through illness, death of loved ones, job loss, economic insecurity, or social isolation, few have escaped the consequences of the worldwide pandemic.
While government and media attention has been focused on physical health, rates of anxiety and depression have soared (1). Younger people have been particularly impacted. One recent study found half of those surveyed were at risk for major depression (2). Such findings have been confirmed in a soon-to-be published study of data generated by practitioners using the ORS and SRS to monitor the care being provided to thousands of adults, adolescents, and children around the world. Briefly, an international group of researchers and scholars found a trend toward increasing episodes of longer lengths of overall less effective care among adolescents and younger adults.
In the US, regardless of client age, therapists are struggling to keep up with demand for mental health services. It’s not a new problem. It’s one that has worsened significantly since the outbreak of COVID-19 (3, 4).
In this environment of demand exceeding availability, it has become increasingly common for clinicians to both: (1) carry higher caseloads; and (2) deliver services on an attenuated schedule for returning clients. Said another way, clinicians are seeing more people, but not the same ones from week to week. Instead, the sessions of those already in care are being spaced further apart so that new intakes can be accommodated (5).
While such developments are entirely understandable in the present environment, the question is whether they constitute sound clinical practice? And where therapeutic effectiveness is concerned, the answer is an unequivocal, “no.” Despite quantity (e.g., number of sessions) not being correlated with outcome, studies do show a clear relationship between frequency and effectiveness — specifically, faster rates of change, improved chances of recovering sooner, and lower rates of attrition (6, 7, 8, 9).
Mindful of such findings, is there anything practitioners and agencies can do to more effectively balance demand with availability? Here, research indicates the answer is, “yes.”
Over the last decade, data have been gathered about the progress of millions of clients via the routine administration of standardized outcome measures. As readers of this already blog know, studies show using the resulting information to adjust services to better fit the individual (aka, Feedback-Informed Treatment) improves retention and outcome while also reducing costs (click here to access a spreadsheet containing a current list of studies).
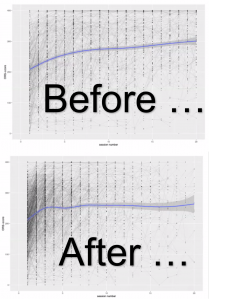
Importantly, the very same data is providing therapists and clients with detailed, evidence-based guidance for optimizing the frequency, dose and intensity of services. As all clinicians know, some clients need and benefit from more, other less. With demand at historically high rates, being able to determine which is which enables practitioners to utilize their limited availability wisely, ensuring maximal improvement for each individual client (10).
If you are interested in learning more, join me and the faculty at the International Center for Clinical Excellence for the next Feedback-Informed Treatment Intensive Trainings. As has been the case since the pandemic first began, this year’s events are entirely online. For more information or to register, click the icons below.
In the meantime, all the best for the Holiday season,
Scott
Scott D. Miller, Ph.D.
Director, International Center for Clinical Excellence



Leave a Reply