
Despite happening decades ago, I remember it as though it were yesterday.
My oldest, Kirk, was fiddling with a cassette tape recorder. He was four at the time and wanted to listen to “his music.” You know, the kind all parents regret having given to their kids at some point? “Wheels on the bus,” “B.I.N.G.O.,” “Itsy bitsy spider.”
Unfortunately, neither the tape or machine were cooperating. Seated at the kitchen table watching, I marveled at his patience and persistence — over and over, inserting the cassette one way, then another.
Eventually, he set the tape down, folded his arms and closed his eyes. That’s when I decided to intervene. I stood and went to sit beside him.
“Hey bud,” I said, gently placing a hand on his knee, “What’s going on?”
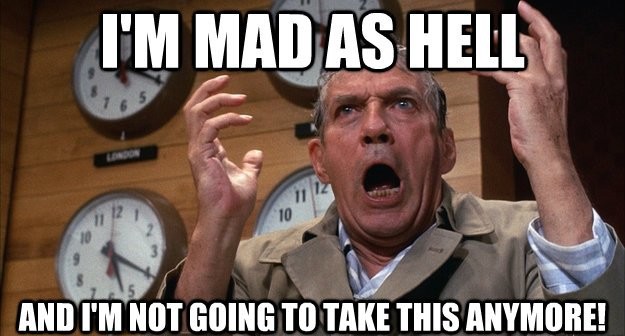
“I … AM … MAD!” he responded slowly and deliberately.
His tone took me by surprise. Kirk was such an even-tempered kid. Rarely upset. Stoic, even when provoked. And I’ll let you in on a little secret. As his father, it was a trait I was proud of, told people about and privately believed he’d learned from me!
Anyway, last week, Kirk and I were on the phone together. I was telling him about an article I’d just published (1). Somewhere along the way, I expressed my frustration with the field of mental health. In particular, our habit of apeing our much-envied and more successful cousins in medicine. So, like them, we insisted on calling our work, “treatment,” likened our methods to taking a pill containing ingredients specifically remedial to a client’s problem. We even adopted a manual developed by physicians defining both the nature and scope of concerns falling within our purview!
Kirk didn’t miss a beat. Teasingly, he asked, “You mean, you … are … MAD?!”
We laughed for several minutes after that, reliving the events from so long ago. Truth is though, I was mad. As my colleague and mentor, Bruce Wampold and I had written in the article (1), our field was at it again, not only adopting the language and terms of medicine, but also implying that field was responsible for the clinical innovation developed by therapists and documented to improve retention and outcome of mental health services (2).
You know what I’m talking about, right?
Regardless of the name it is known by (e.g., feedback-informed treatment, routine outcome monitoring, patient focused research, progress feedback, or practice based evidence) research on the subject originated with non-medical mental health researchers and has been going on for a quarter century (3)! And yet, in proposing “practice guidelines” for the American Psychological Assocation, Boswell and colleagues (3), opted for a term developed by a physician in 2006, “measurement-based care” (MBC) (4), claiming it was “closely related, though not necessarily identical to, commonly used terms/practices” noted above (p. 3).
Judge for yourself. Here’s how the authors defined MBC: “(a) routinely collecting patient-generated data throughout the course of treatment; (b) sharing timely feedback with the patient about these data (e.g., patient-reported outcome measure scores) and observed or predicted trends over time to engage patients in their treatment; and (c) acting on these data in the context of the provider’s clinical judgment and the patient’s experiences” (p. 3). Now, compare that to the definition of feedback-informed treatment offered in the FIT Treatment and Training Manuals published years earlier. “FIT is a pantheoretical approach for evaluating and improving the quality and effectiveness of behavior health services. It involves routinely and formally soliciting feedback from consumers regarding the therapeutic alliance and outcome of care and using the resulting information to inform and tailor service delivery” (p. 2).
If the two definitions seem similar, its because they are!
(Sorry for my tone)
Beyond once again emulating medicine, the problem with the term, “measurement-based care,” is that it doesn’t capture what the authors claim it represents. Indeed, wouldn’t the average practitioner on first hearing be most inclined to conclude the point of MBC is, well, measurement? That is precisely the confusion I encounter weekly in emails, phone calls and consultations with mental health professionals, agency managers, and payers.
“Please don’t use my scales,” I generally advise. Their response? Always a but …
“We’ve been told by [our payer, funder, the government, some regulatory body] that we have to use an outcome scale?”
“How will I know if the therapists who work at my agency are effective?”
“We need a way to identify clients we aren’t helping so we can terminate services with them and free up scarce clinical resources.”
Returning to my son, Kirk. On closer examination, it turned out a small part in the compartment of the recorder designed to hold the tape had broken off. Nothing we could do at that point would make it work.
“It’s OK, Dad,” I recall him saying, then quickly adding, “we can sing the songs ourselves.”
What could I say? We did.
It’s time, I think, our field does the same.
All the best,
Scott
Scott D. Miller, Ph.D.
Director, International Center for Clinical Excellence


Measurement based care is becoming a catch phrase in Ontario, Canada as well. Undoubtedly influenced by the emergence of this idea in the USA. I try to educate my colleagues and management about these issues and point out that FIT originated in the field of psychotherapy and has been appropriated (sort of) by our medical colleagues. I was surprised to see the American Psychological Association’s use of the term instead of FIT. As you’ve noted, the profession of psychology has all too often tried to emulate the field of medicine. It is much the same in Canada.
BTW, I greatly appreciate the story about your son, especially the outcome.
Best regards,
Roy
Scott, this is brilliant. I love the story of you and your son too.
I worry that one of the unintended consequences is that we end up creating “performance” systems and not dynamic learnings systems in our clinical practice.
Scott, I admire your patience in researching, writing & teaching for decades that psychotherapy is not analogous to the medical model where we can use measurements as a one-size fits all basis of treatment.
The FIT scales are about giving the clients a voice in their treatment, plus giving the therapists useful feedback to tailor our work to each client. It’s no doubt that Kirk learnt his Stoicism from you 🙂 But Stoics are not emotionless robots as most people assume. After all your efforts, being MAD at Boswell & colleagues for co-opting the much more elegant definition of FIT for behavioural health treatments seems human & understandable.