Get ready. The revolution is coming (if not already here). Whether you are a direct service provider (psychologist, counselor, marriage and family therapist), agency, broker, or funder, you will be required to measure and likely report the outcomes of your clinical work.
.jpg)
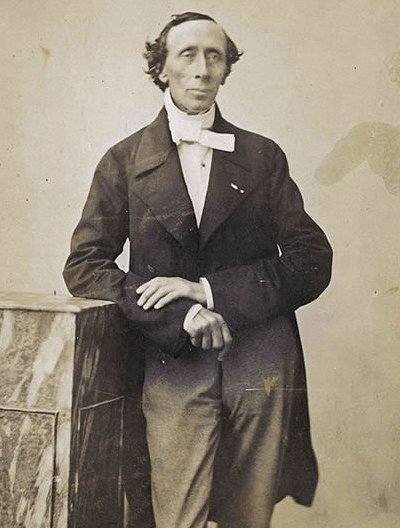
Jay Lebow, Ph.D.
Just this month, Dr. Jay Lebow, a professor of psychology at the Family Institute at Northwestern University, published an article in the Psychotherapy Networker–the most widely circulated publication for practitioners in the world–where he claimed the field had reached a “tipping point.” “Once a matter of interest only among a small circle of academics,” Dr. Lebow writes in his piece entitled, The Big Squeeze, “treatment outcome has now become a part of the national debate about healthcare reform.”
.jpg)
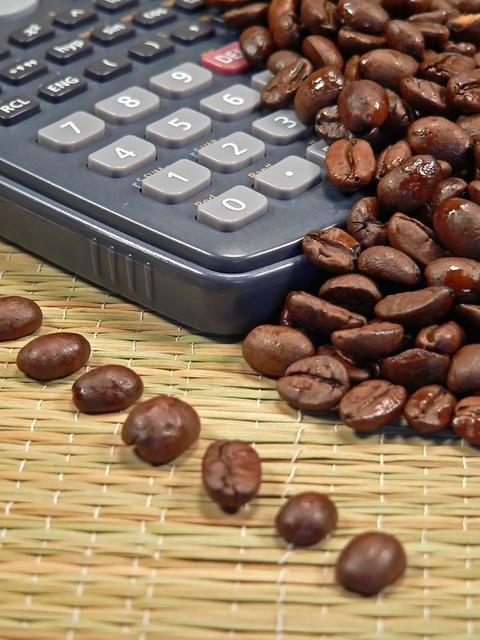
David Barlow, Ph.D.
The same sentiments were expressed in a feature article entitled, “Negative Effects from Psychological Treatments,” written by Dr. David Barlow in the January issue of the American Psychologist. “Therapists,” he argues both eloquently and persuasively, “do not have to wait for the next clinical trial….[rather] clinicians [can act] as local clinical scientists…[using] outcome measures to track progress…rapidly becom[ing] aware of lack of progress or even deterioration” (p. 19). What can I say, except that any practitioner with more than a few years to work before retirement, should read these articles and then forward them to every practitioner they know.
During the Holidays, and just before the turn of the New Year, I blogged about the trend toward outcome measurement. As readers will recall, I talked about my experience on a panel at the Evolution of Psychotherapy conference where Dr. Barlow–who, in response to my brief remarks about the benefits of feedback– suprised me by stating unequivocally that all therapists would soon be required to measure and monitor the outcome of their clinical work. And even though my work has focused almost exclusively on measuring and using outcomes to improve both retention in and the results of behavioral health for the last 15 years, I said his pronouncement frightened me–which, by the way, reminds me of a joke.
A sheep farmer is out in the pasture tending his flock–I promise this is clean, so read on–when from over a small hill comes a man in a custom-tailored, three-piece business suit. In one hand, the businessman holds a calculator; in the other, an expensive, leather brief case. “I have a proposition for you,” the well-clad man says as he approaches the farmer, and then continues, “if I can tell you how many sheep are in your flock, to the exact number, may I have one of your sheep?” Though initially startled by the stranger’s abrupt appearance and offer, the farmer quickly gathers his wits. Knowing there is no way the man could know the actual number of sheep (since many in his flock were out of site in other pastures and several were born just that morning and still in the barn), the farmer quickly responded, “I’ll take that bet!”

Without a moment’s hesitation, the man calls out the correct number, “one thousand, three hundred and forty six,” then quickly adds, “…with the last three born this morning and still resting in the barn!” Dumbfounded, the farmer merely motions toward his flock. In response, the visitor stows his calculator, slings one of the animals up and across his shoulders and then, after retrieving his briefcase, begins making his way back up the hill. Just as he nears the top of the embankment, the farmer finds his voice and calls out, “Sir, I have a counter proposal for you.”
“And what might that be?” the man replies, turning to face the farmer, who then asked, “If I can tell you, sir, what you do for a living, can I have my animal back?”
Always in the mood for a wager, the stranger replies, “I’ll take that bet!” And then without a moment’s hesitation, the sheep farmer says, “You’re an accountant, a bureaucrat, a ‘bean-counter.'” Now, it’s the businessman’s turn to be surprised. “That’s right!” he says, and then asks, “How did you know?”
“Well,” the farmer answers, “because that’s my dog you have around your neck.”
The moral of the story? Bureaucrats can count but they can’t tell the difference between what is and is not important. In my blogpost on December 24th, I expressed concern about the explosion of “official interest” in measuring outcomes. As the two articles mentioned above make clear, the revolution has started. There’s no turning back now. The only question that remains is whether behavioral health providers will be present to steer measurement toward what matters? Here, our track record is less than impressive (remember the 80-90’s and the whole managed care revolution). We had ample warning (and did, well, nothing. If you don’t believe me, click here and read this article from 1986 by Dr. Nick Cummings).
As my colleague and friend Peter Albert is fond of saying, “If you’re not at the table, you’re likely to be on the menu.” So, what can the average clinician do? First of all, if you haven’t already done so, began tracking your outcomes. Right here, on my website, you can download, free, simple-to use, valid and reliable measures. Second, advocate for measures that are feasible, client-friendly, and have a empirical track record of improving retention and outcome. Third, and lastly, join the International Center for Clinical Excellence. Here, clinicians from all over the globe are connecting, learning, and sharing their experiences about how to use ongoing measures of progress and alliance. Most importantly, all are determined to lead the revolution.

.jpg)


.jpg)
.jpg) Researchers
Researchers 

.jpg)
.jpg)