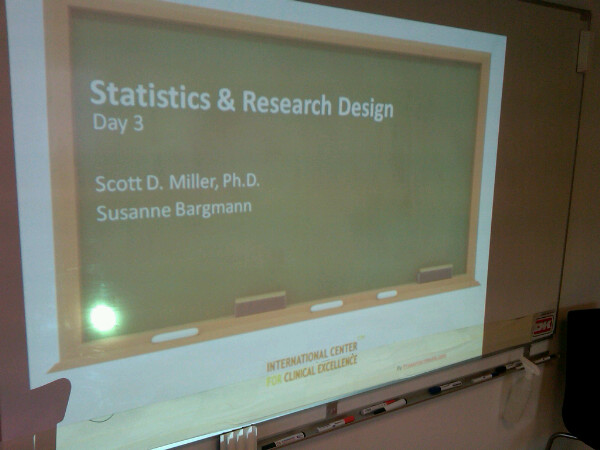
Horsholm, Denmark
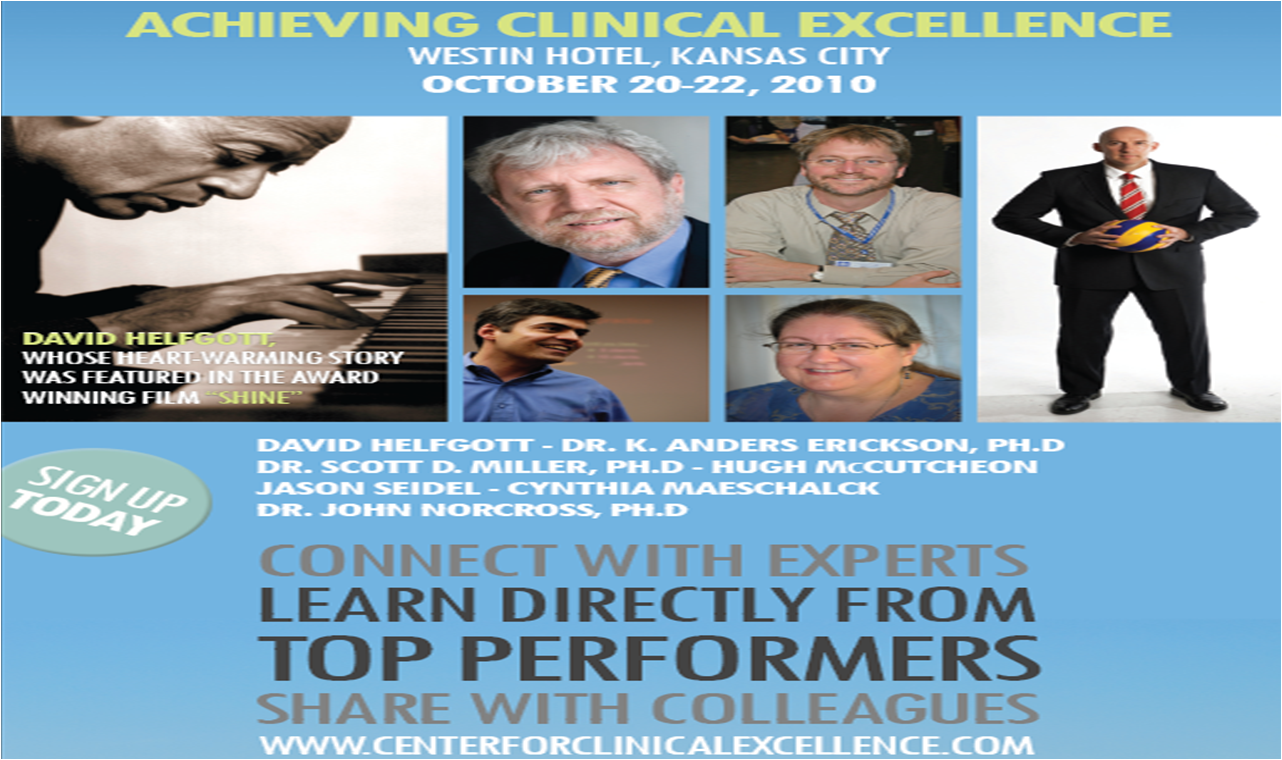
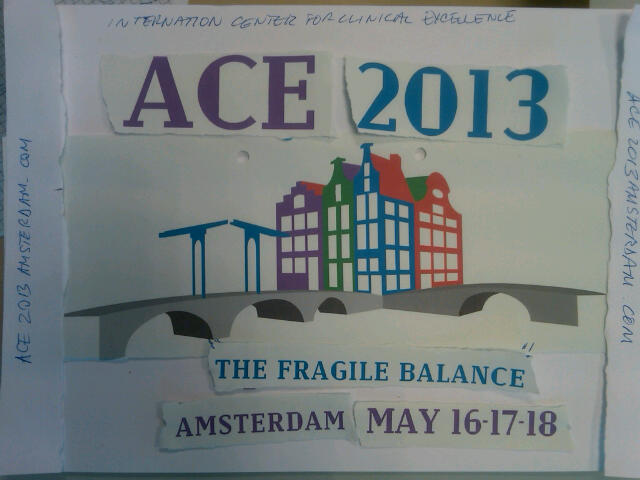
Spent the weekend with the planning committe for the 2013 Achieving Clinical Excellence Conference. Committee members came in from all over the world–the USA, Romania, Holland, the UK, and Denmark–to finalize speakers, the conference venue, and mock up the logo for the conference brochure and advertizing. Like last time, we are not only bringing in the top researchers to present the latest scientific findings, but also superior performers from a variety of vocations to inspire all of us to achieve our personal best.
Despite all the effort, a significant part of the program remains incomplete. That part involves YOU! The conference committee is issuing a formal “call for papers”on expertise and expert performance in the field of behavioral health. In keeping with the theme of the conference–“Putting the Pieces Together: The Fragile Balance”–the committe is looking for presentations on:
- Innovative strategies for improving the quality and outcome of behavioral health;
- Research and experiences of using routine monitoring of progress and the alliance to improve retention and outcome of treatment services;
- Principles, practices, and experiences regarding maintaining balance between professional and personal life in the achievement of clinical excellence;
- Implementation of strategies for improving performance in agencies and systems of care
- How professional development can improve performance of behavioral health professionals;
- Management and leadership practices associated with superior performance in behavioral health;
Any and all papers may be submitted directly to: info@scottdmiller.com. The conference website is also available for earlybird registration.
There are so many other developments that I hope to blog in detail about in the coming days. In the meantime, here’s a short summary of what’s in store:


.png)
.png)






.jpg)


.jpg)
.jpg)









.jpg)
.jpg)








.gif)


.jpg)