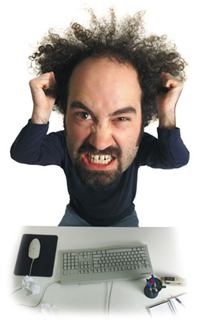
So what do the data actually say? S adly, the answer is often, “it depends on who you ask.” If you read the latest summary and treatment recommendations for post-traumatic stress disorder (PTSD) posted by the Cochrane Collaboration, you are told that TFCBT and EMDR are the most effective, “state of the art” treatments on offer. Other summaries, as I recently blogged about, arrive at very—even opposite—conclusions; namely, all psychotherapies (trauma-focused and otherwise) work equally well in the treatment of PTSD. For the practicing clinician (as well as other consumers of research), the end result is confusion and, dare I say, despair.
Unable to resolve the discrepant findings, the research is either rejected out of hand (“it’s all crap anyway”) or cherry-picked (“your research is crap, mine is good”). In a world where experts disagree–and vehemently–what is the average Joe or Jane therapist to do?
Fortunately, there is another way, beyond agnosticism and instead of fundamentalism. In a word, it is engagement. This last week, I spent 5 days teaching an intensive workshop with ICCE Senior Associate Susanne Bargmann to a group of Danish psychologists on “Statistics and Research Design.” That’s right. Five days, 6 hours a day spent away from work and clients learning how to understand, read, and conduct research.

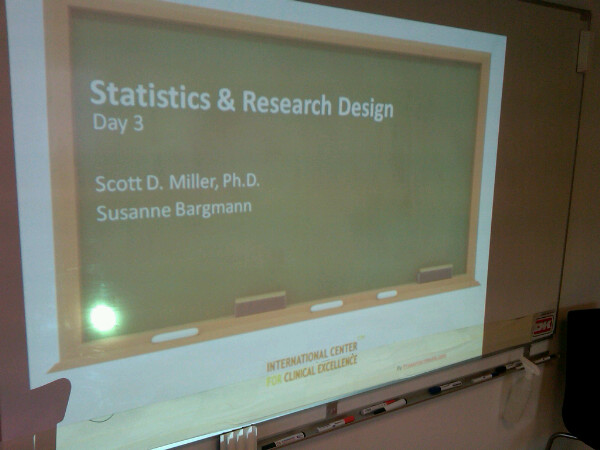

The goal of the training was simple and straight-forward: help practitioners learn to evaluate the methods and meanings, strengths and weaknesses, and political and paradigmatic influences associated with research and evidentiary claims. At the conclusion of the five days, none of those assembled had difficulty engaging with and understanding the reasons for the seemingly discrepant findings noted above. As a result, they could state with confidence “what works” with PTSD, helping clarify this not only to colleagues, payers, and policy members but also to consumers of behavioral health services.
The “Statistics and Research Design” course will be held again in Denmark in 2011. If the experience of this year’s participants proves anything, it is that, “The only thing therapists have to fear about statistics and research design, is fear itself.” Please contact Vinther and Mosgaard directly for more information.
Finally, as part of the International Center for Clinical Excellence (ICCE) efforts to improve the quality and outcome of behavioral health services worldwide, two additional intensive trainings will be offered in Chicago, Illinois (USA). First, the “Advanced Training in Feedback-Informed Treatment (FIT).” And second, the annual “Training of Trainers.” In the Advanced Training, participants learn:

.jpg)





.gif)




.jpg)