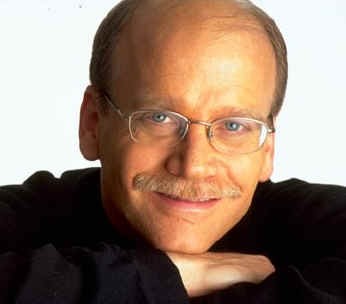
 John Norcross, Ph.D. is without a doubt the researcher that has done the most to highlight the evidence-base supporting the importance of the relationship between clinician and consumer in successful behavioral healthcare. The second edition of his book, Psychotherapy Relationships that Work, is about to be released. Like the last edition, this volume is a virtual treasure trove of research findings and empirically supported practices.
John Norcross, Ph.D. is without a doubt the researcher that has done the most to highlight the evidence-base supporting the importance of the relationship between clinician and consumer in successful behavioral healthcare. The second edition of his book, Psychotherapy Relationships that Work, is about to be released. Like the last edition, this volume is a virtual treasure trove of research findings and empirically supported practices.
.jpg)
Among the many gems in the book is a chapter by Michael J. Lambert, Ph.D–pioneering researcher on “feedback-informed treatment” (FIT). As usual, he does a masterful job summarizing the existing research on the subject. The data are overwhelmingly positive: seeking and using standardized feedback regarding the progress and outcome of treatment cuts drop out and deterioration rates and significantly improves outcome.
Lambert also reports the results of two meta-analyses. One performed on studies using his own OQ System family of measures, the other based on research using the ORS and SRS. Not only did he find ample empirical support for the two systems, but in the case of the ORS and SRS those therapies informed by feedback, “had 3.5 times higher odds of experiencing reliable change.” Additionally, and importantly, the brief, 4-item ORS and SRS scales performed the same as the longer and more detailed OQ 45.2.
What can you do? First, order John’s book. Second, if you are not FIT, now is the time to register to use the measures. And if you need support, why not join the International Center for Clinical Excellence? Like the measures, there is no cost. Right now, professionals from different disciplines, working in diverse settings are connecting with and learning from each other. Here’s a nudge: you’ll be able to reach John Norcross there—he’s one of ICCE’s newest members.





.jpg)
